The Pickleball Injury Surge: What Every Player Should Know
Pickleball has taken the country by storm. With courts popping up in neighborhoods, clubs, and rec centers across the U.S., it’s no surprise that this fast-paced sport has become a favorite for all age groups. But with rising popularity comes a notable spike in injuries—particularly among older players.
A recent study using data from the National Electronic Injury Surveillance System (NEISS) revealed over 53,000 pickleball-related injuries between 2012 and 2021. While players of all ages are getting hurt, the nature of these injuries—and how to prevent them—varies significantly by age.
Let’s break down what the research says and what you can do to stay safe and strong on the court.
Key Findings: Injury Patterns by Age
The data shows clear differences in how younger and older pickleball players get injured:
Older Players (Ages 65+):
- 83% of all injuries occurred in this age group.
- Most injuries were due to slips, trips, falls, or dives.
- Fractures were the most common injury, especially in the wrist, hip, and shoulder.
- Older players were nearly three times more likely to suffer fractures than younger players.
Younger Players (<65):
- Although younger players made up a smaller percentage of injuries, their injury rate is increasing rapidly.
- More likely to experience strains and sprains, especially to the shoulders, knees, and lower back.
- Injuries were often caused by dynamic movements like lunging, twisting, or stopping suddenly.
Why Are Injuries on the Rise?
Pickleball is deceptively demanding. Its small court size, rapid direction changes, and repetitive swinging motions challenge both joint stability and muscle control. While it offers a great cardiovascular workout, players often underestimate the need for proper warm-up, conditioning, and mobility.
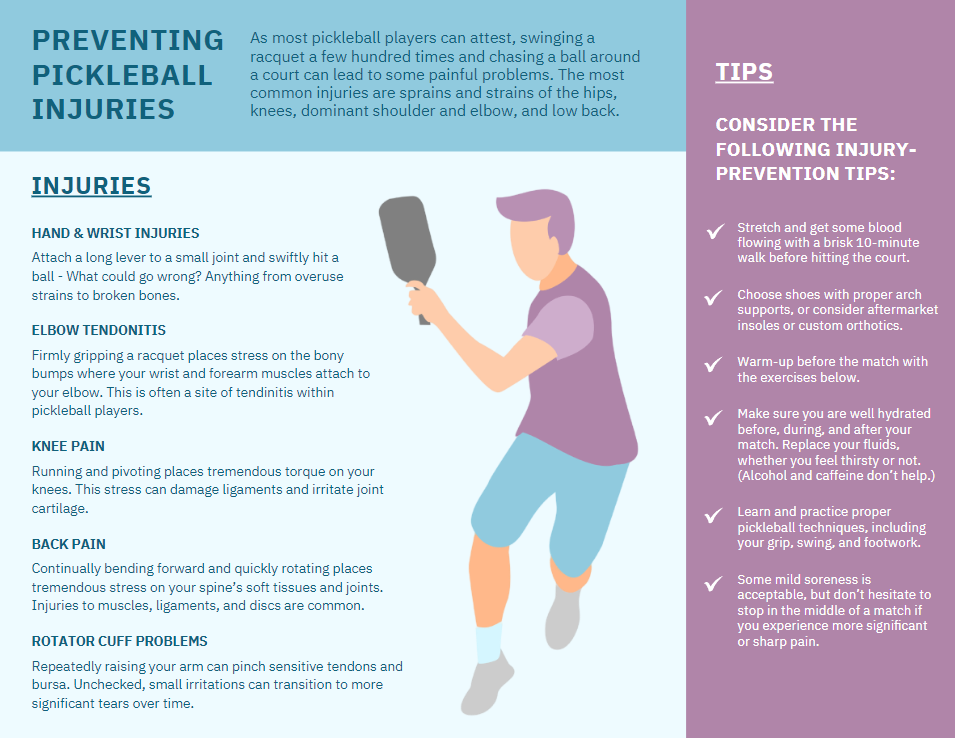
Common Pickleball Injuries We See in Clinic
At our practice, we frequently treat pickleball-related injuries, including:
- Rotator cuff irritation and tears
- Tennis elbow (lateral epicondylitis)
- Knee ligament strains
- Low back pain and muscle spasms
- Wrist fractures or overuse injuries
- Hamstring and calf strains
Whether you're a recreational weekend player or a competitive tournament regular, these injuries can quickly sideline you.
Prevention Strategies for All Ages
For Older Adults:
- Improve balance and proprioception. Targeted exercises can reduce the risk of falls and fractures.
- Strengthen supporting muscles. Focus on hip and core stability to stay steady during lateral movement.
- Maintain bone health. Talk to your provider about bone density screening and fall prevention strategies.
- Check footwear. Grippy, supportive shoes can reduce fall risk on court surfaces.
For Younger Adults:
- Warm up properly. Dynamic stretches and light cardio help prepare joints and muscles for play.
- Focus on mobility. Tight hips, shoulders, and hamstrings are a recipe for strain injuries.
- Cross-train. Strength training can enhance joint support and reduce stress on connective tissue.
- Don’t play through pain. Early treatment prevents small injuries from becoming chronic issues.
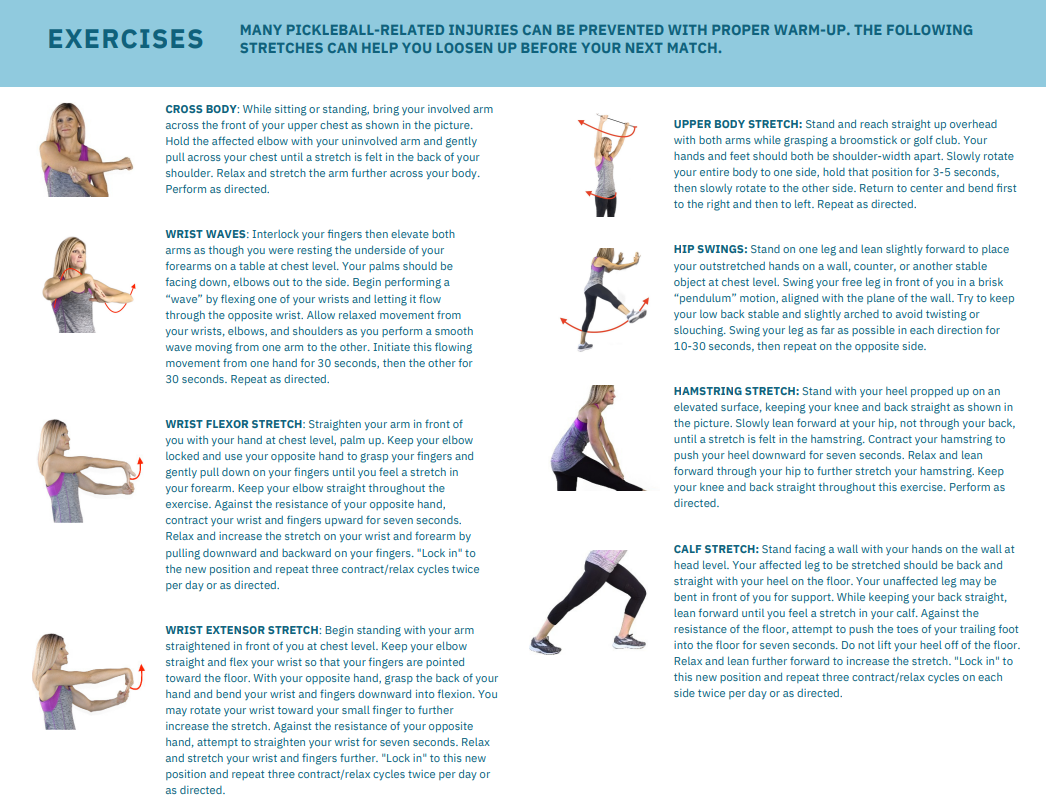
Try These Warm-Up Stretches Before Your Next Match
Start every session with a 5–10 minute warm-up. Here are a few clinic-approved movements:
- Wrist Waves – Loosen the small joints in your forearms and wrists before repetitive swinging.
- Cross-Body Shoulder Stretch – Improves shoulder mobility and prepares the rotator cuff.
- Hip Swings – Activates your hip flexors and hamstrings for better court movement.
- Upper Body Twists with Broomstick – Enhances thoracic spine mobility and rotation.
- Calf and Hamstring Stretches – Reduces the chance of muscle pulls during lunges or sprints.
We recommend pairing these stretches with light resistance or bodyweight exercises to build joint stability over time.
Don’t Wait Until You’re Injured
Pickleball is here to stay, and that’s a good thing. It promotes activity, social connection, and longevity. But if you're dealing with stiffness, joint pain, or a nagging injury that’s affecting your game, don’t ignore it.
At Thrive, we provide:
- Sports chiropractic care
- Soft tissue therapy
- Joint mobilization
- Injury prevention screenings
- Customized exercise programs for pickleball players of all levels
Ready to Stay in the Game?
Don’t let pain keep you off the court. Whether you’re just picking up the paddle or playing competitively, our team can help you move better, recover faster, and prevent future injuries.
Source: Injury surveillance data from the National Electronic Injury Surveillance System (NEISS), 2021.
Citation:
Orthop J Sports Med. 2025 Jan 23;13(1):23259671241305364. doi: 10.1177/23259671241305364